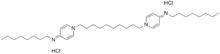
Octenidine dihydrochloride
Octenidine dihydrochloride is a cationic surfactant, with a gemini-surfactant structure, derived from pyridine. It is active against Gram-positive and Gram-negative bacteria. Since 1987, it has been used primarily in Europe as an antiseptic prior to medical procedures, including on neonates.
 | |
| Names | |
|---|---|
| IUPAC name
N-octyl-1-[10-(4-octyliminopyridin-1-yl)decyl]pyridin-4-imine dihydrochloride | |
| Systematic IUPAC name
N,N'-(decane-1,10-diyldipyridin-1-yl-4-ylidene)dioctan-1-amine dihydrochloride | |
| Other names
N,N'-(decane-1,10-diyldi-1(4H)-pyridyl-4-ylidene)bis(octylammonium) dichloride | |
| Identifiers | |
| |
3D model (JSmol) |
|
| ChEBI | |
| ChEMBL | |
| ChemSpider | |
| ECHA InfoCard | 100.068.035 |
| EC Number |
|
PubChem CID |
|
| UNII |
|
CompTox Dashboard (EPA) |
|
| |
| |
| Properties | |
| C36H64Cl2N4 | |
| Molar mass | 623.84 g·mol−1 |
| Pharmacology | |
| R02AA21 (WHO) combination codes: D08AJ57 (WHO) G01AX66 (WHO) | |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
| Infobox references | |
Use
Since 1987, octenidine has been used in Europe as an antiseptic, in concentrations of 0.1 to 2.0%. It is a substitute for chlorhexidine, with respect to its slow action and concerns about the carcinogenic impurity 4-chloroaniline. Octenidine preparations are less expensive than chlorhexidine and no resistance had been observed as of 2007.[2] They may contain the antiseptic phenoxyethanol.[3] It is not listed in the Annex V of authorized preservatives of the European Cosmetic Regulation 1223/2009.
Efficacy
Octenidine dihydrochloride is active against Gram-positive and Gram-negative bacteria.[4]
In vitro suspension tests with 5 minute exposure time have shown that octenidine requires lower effective concentrations than chlorhexidine to kill common bacteria like Staphylococcus aureus, Escherichia coli, Proteus mirabilis and the yeast Candida albicans.[5]
| Effective concentration, % | ||
|---|---|---|
| Octenidine dihydrochloride | Chlorhexidine digluconate | |
| Staphylococcus aureus | 0.025 | >0.2 |
| Escherichia coli | 0.025 | 0.1 |
| Proteus mirabilis | 0.025 | >0.2 |
| Candida albicans | 0.01 | 0.025 |
| Pseudomonas aeruginosa | 0.025 | >0.2 |
An observational study of using octenidine on the skin of patients in 17 intensive care units in Berlin in 2014 showed decreasing nosocomial infection rates.[6]
In a survey of German neonatal intensive-care units octenidine without phenoxyethanol and octenidine were the most common skin antiseptics used for intensive-care procedures. Skin complications included blistering, necrosis and scarring, which has not been previously reported in this population.[3]
In a 2016 study of pediatric cancer patients with long-term central venous access devices using octenidine/isopropanol for the disinfection of catheter hubs and 3-way stopcocks as part of a bundled intervention, the risk of bloodstream infections decreased.[7]
Safety
Octenidine is absorbed neither through the skin, nor through mucous membranes, nor via wounds and does not pass the placental barrier. However, cation-active compounds cause local irritation and are extremely poisonous when administered parenterally.[5]
In a 2016 in vitro study of mouth rinses on gingival fibroblasts and epithelial cells octenidine showed a less cytotoxic effect, especially on epithelial cells, compared to chlorhexidine after 15 min.[8] Wound irrigation with octenidine has caused severe complications in dogs,[9] aseptic necrosis and chronic inflammation in penetrating hand wounds.[10]
References
- EC no. 274-861-8, ECHA
- Al-Doori Z, Goroncy-Bermes P, Gemmell C et al. Low-level exposure of MRSA to octenidine dihydrochloride does not select for resistance. J Antimicrob Chemother 2007; 59: 1280–1.
- Biermann CD1, Kribs A1, Roth B1, Tantcheva-Poor I2 (2016). "Use and Cutaneous Side Effects of Skin Antiseptics in Extremely Low Birth Weight Infants - A Retrospective Survey of the German NICUs". Klinische Pädiatrie. 228 (4): 208–12. doi:10.1055/s-0042-104122. PMID 27362412.CS1 maint: multiple names: authors list (link)
- Sedlock D, Bailey D. Microbicidal activity of octenidine hydrochloride, a new alkanediylbis[pyridine] germicidal agent. Antimicrob Agents Chemother. 1985; 28: 786–90.
- Hans-P. Harke (2007), "Disinfectants", Ullmann's Encyclopedia of Industrial Chemistry (7th ed.), Wiley, pp. 1–17, doi:10.1002/14356007.a08_551
- Gastmeier P, Kämpf K, Behnke M, Geffers C, Schwab F (2016). "An observational study of the universal use of octenidine to decrease nosocomial bloodstream infections and MDR organisms". Journal of Antimicrobial Chemotherapy. 71 (9): 2569–76. doi:10.1093/jac/dkw170. PMID 27234462.
- Furtwängler, Rhoikos; Laux, Carolin; Graf, Norbert; Simon, Arne (2015). "Impact of a modified Broviac maintenance care bundle on bloodstream infections in paediatric cancer patients". GMS Hygiene and Infection Control. 10: Doc15. doi:10.3205/dgkh000258. PMC 4657435. PMID 26605135.
- Schmidt, J.; Zyba, V.; Jung, K.; Rinke, S.; Haak, R.; Mausberg, R. F.; Ziebolz, D. (2016). "Cytotoxic effects of octenidine mouth rinse on human fibroblasts and epithelial cells – anin vitrostudy". Drug and Chemical Toxicology. 39 (3): 322–330. doi:10.3109/01480545.2015.1121274. PMID 26654138. S2CID 19546288.
- Kaiser, S.; Kramer, M.; Thiel, C. (2015). "Severe complications after non-intended usage of octenidine dihydrochloride. A case series with four dogs". Tierärztliche Praxis. Ausgabe K, Kleintiere/Heimtiere. 43 (5): 291–298. doi:10.15654/TPK-150029. PMID 26353826.
- Lachapelle JM (2014). "A comparison of the irritant and allergenic properties of antiseptics". European Journal of Dermatology. 24 (1): 3–9. doi:10.1684/ejd.2013.2198. PMID 24492204.