Testicular pain
Testicular pain, also known as scrotal pain, occurs when part or all of either one or both testicles hurt. Pain in the scrotum is also often included. Testicular pain may be of sudden onset or of long duration.[1][2]
| Testicle pain | |
|---|---|
| Other names | Scrotal pain, orchialgia |
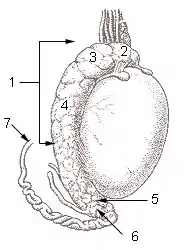 | |
| 1 - 6: Epididymis 7: Vas deferens | |
| Specialty | Urology |
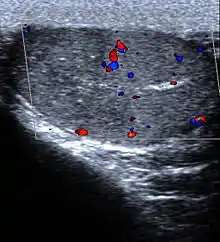
| Diagnostic method | Ultrasound, urine tests, blood tests[1][2] |
| Differential diagnosis | Acute: Epididymitis, testicular torsion, testicular cancer, varicocele, Fournier gangrene[1] Chronic: Varicocele, spermatocele, Henoch–Schönlein purpura, post-vasectomy pain syndrome, chronic pelvic pain syndrome[2] |
Causes range from non serious muscular skeletal problems to emergency conditions such as Fournier gangrene and testicular torsion. The diagnostic approach involves making sure no serious conditions are present. Diagnosis may be supported by ultrasound, urine tests, and blood tests.[1][2]
Pain management is typically given with definitive management depending on the underlying cause.
Definition
Testicular pain is when part or all of either one or both testicles hurt. Pain of the scrotum is often included. It may be either acute, subacute or chronic depending on its duration.
Chronic scrotal pain
Chronic scrotal pain (pain for greater than 3 months) may occur due to a number of underlying conditions.[3] It occurs in 15-19% of men post vasectomy, due to infections such as epididymitis, prostatitis, and orchitis, as well as varicocele, hydrocele, spermatocele, polyarteritis nodosa, testicular torsion, previous surgery and trauma.[3] In 25% of cases the cause is never determined.[3] The pain can persist for a long and indefinite period of time following the vasectomy, in which case it is termed post-vasectomy pain syndrome (PVPS).
Differential diagnosis
The differential diagnosis of testicular pain is broad and involves conditions from benign to life-threatening. The most common causes of pain in children presenting to the emergency room are testicular torsion (16%), torsion of a testicular appendage (46%), and epididymitis (35%).[4] In adults, the most common cause is epididymitis.
Testicular torsion
Testicular torsion usually presents with an acute onset of diffuse testicular pain and tenderness of less than 6 hrs of duration. There is often an absent or decreased cremasteric reflex, the testicle is elevated, and often is horizontal.[5] It occurs annually in about 1 in 4,000 males before 25 years of age,[3] is most frequent among adolescents (65% of cases presenting between 12 – 18 years of age),[6] and is rare after 35 years of age.[7] Because it can lead to necrosis within a few hours, it is considered a surgical emergency.[7] Another version of this condition is a chronic illness called intermittent testicular torsion (ITT) which is characterized by recurrent rapid acute onset of pain in one testis which will temporarily assume a horizontal or elevated position in the scrotum similar to that of a full torsion followed by eventual spontaneous detortion and rapid solution of pain. Nausea or vomiting may also occur.[8]
Epididymitis and orchitis
Epididymitis occurs when there is inflammation of the epididymis (a curved structure at the back of the testicle).[7] This condition usually presents with gradual onset of varying degrees of pain, and the scrotum may be red, warm and swollen. It is often accompanied by symptoms of a urinary tract infection, fever, and in over half of cases it presents in combination with orchitis.[7] In those between the ages of 14 to 35 it is usually caused by either gonorrhea or chlamydia. In people either older or younger E. coli is the most common bacterial infection.[7] Treatment involves the use of antibiotics.[7]
Fournier's gangrene
Fournier's gangrene (an aggressive and rapidly spreading infection of the perineum) usually presents with fever and intense pain. It is a rare condition but fatal if not identified and aggressively treated with a combination of surgical debridement and broad spectrum antibiotics.[9]
Others
Many other less common conditions can lead to testicular pain. These include inguinal hernias, injury, hydroceles, degenerative disease of lumbar spine,[10] disc herniations,[11] and varicoceles among others. Testicular cancer is usually painless.[12] Another potential cause is epididymal hypertension (also known as "blue balls").[13]
Diagnostic approach
Physical findings
The cremaster reflex (elevation of the testicle in response to stroking the upper inner thigh) is typically present in epididymitis but absent in testicular torsion as the testis is already elevated.[7] Prehn's sign (the relief of pain with elevation) though a classic physical exam finding has not been found to be reliable in distinguishing torsion from other causes of testicular pain such as epididymitis.[14]
Laboratory tests
Useful tests that may help in the determination of the cause include a urinalysis (usually normal in testicular torsion). Pyuria and bacteriuria (white blood cells and bacteria in the urine) in patients with acute scrotum suggests an infectious cause such as epididymitis or orchitis and specific testing for gonorrhea and chlamydia should be done.[7] All people with chronic pain should be tested for gonorrhea and chlamydia.[3]
References
- Boniface, Michael (16 December 2018). "Acute Scrotum Pain". StatPearls. PMID 29262236.
- Leslie, Stephen (2 May 2019). "Chronic Testicular Pain (Orchialgia)". StatPearls. PMID 29494088.
- Wampler SM, Llanes M (September 2010). "Common scrotal and testicular problems". Prim. Care. 37 (3): 613–26, x. doi:10.1016/j.pop.2010.04.009. PMID 20705202.
- Lewis AG, Bukowski TP, Jarvis PD, Wacksman J, Sheldon CA (February 1995). "Evaluation of acute scrotum in the emergency department". J. Pediatr. Surg. 30 (2): 277–81, discussion 281–2. doi:10.1016/0022-3468(95)90574-X. PMID 7738751.
- Karmazyn B, Steinberg R, Kornreich L, et al. (March 2005). "Clinical and sonographic criteria of acute scrotum in children: a retrospective study of 172 boys". Pediatr Radiol. 35 (3): 302–10. doi:10.1007/s00247-004-1347-9. PMID 15503003. S2CID 25553523.
- Edelsberg JS, Surh YS (August 1988). "The acute scrotum". Emerg. Med. Clin. North Am. 6 (3): 521–46. PMID 3292226.
- Trojian TH, Lishnak TS, Heiman D (April 2009). "Epididymitis and orchitis: an overview". Am Fam Physician. 79 (7): 583–7. PMID 19378875.
- Uribe, Juan F. (2008). Potts, Jeannette M. (ed.). Genitourinary pain and inflammation: diagnosis and management. Totowa, New Jersey: Humana. p. 150. ISBN 978-1-58829-816-4.
- Burch DM, Barreiro TJ, Vanek VW (November 2007). "Fournier's gangrene: be alert for this medical emergency" (PDF). JAAPA. 20 (11): 44–7. doi:10.1097/01720610-200711000-00020. PMID 18035764. S2CID 45641097. Archived from the original (PDF) on 2009-10-07.
- Chu, Eric Chun Pu (8 August 2020). "Taming of the Testicular Pain Complicating Lumbar Disc Herniation With Spinal Manipulation". Am J Mens Health. 2020 Jul-Aug (14): 4. doi:10.1177/1557988320949358. PMC 7418242. PMID 32772625.
- Chu, Eric (7 August 2020). "Taming of the Testicular Pain Complicating Lumbar Disc Herniation With Spinal Manipulation". American Journal of Men's Health. 14 (4). doi:10.1177/1557988320949358. PMID 32772625.
- "Testicle pain: MedlinePlus Medical Encyclopedia". National Institute of Health.
- Chalett JM, Nerenberg LT (October 2000). ""Blue balls": A diagnostic consideration in testiculoscrotal pain in young adults: A case report and discussion". Pediatrics. 106 (4): 843. doi:10.1542/peds.106.4.843. PMID 11015532. S2CID 36966128.
- Lavallee ME, Cash J (April 2005). "Testicular torsion: evaluation and management". Curr Sports Med Rep. 4 (2): 102–4. doi:10.1097/01.CSMR.0000306081.13064.a2. PMID 15763047. S2CID 209145837.
- Galejs LE (February 1999). "Diagnosis and treatment of the acute scrotum". American Family Physician. 59 (4): 817–24. PMID 10068706.
External links
| Classification | |
|---|---|
| External resources |