Autosomal dominant retinal vasculopathy with cerebral leukodystrophy
Autosomal Dominant Retinal Vasculopathy with Cerebral Leukodystrophy (AD-RVCL) (previously known also as Cerebroretinal Vasculopathy, CRV, or Hereditary Vascular Retinopathy, HVR or Hereditary Endotheliopathy, Retinopathy, Nephropathy, and Stroke, HERNS) is an inherited condition resulting from a frameshift mutation to the TREX1 gene. This genetically inherited condition affects the retina and the white matter of the central nervous system, resulting in vision loss, lacunar strokes and ultimately dementia. Symptoms commonly begin in the early to mid-forties, and treatments currently aim to manage or alleviate the symptoms rather than treating the underlying cause. The overall prognosis is poor, and death can sometimes occur within 10 years of the first symptoms appearing.[1]
| Autosomal dominant retinal vasculopathy with cerebral leukodystrophy | |
|---|---|
| Other names | Retinal vasculopathy and cerebral leukoencephalopathy |
 | |
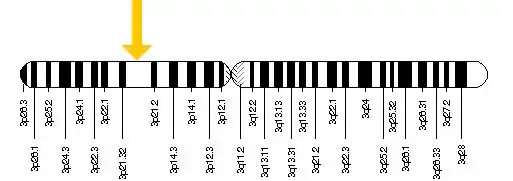
| Diagram depicts the mode of inheritance of this condition | |
Presentation
- No recognizable symptoms until after age 40.
- No environmental toxins have been found to be attributable to the condition.
- The condition is primarily localized to the brain and eyes.
- Optically correctable, but continuous, deterioration of visual acuity due to extensive multifocal microvascular abnormalities and retinal neovascularization leading, ultimately, to a loss of vision.
- Elevated levels of alkaline phosphatase.
- Subtle vascular changes in the retina resembling telangiectasia (spider veins) in the parafovea circulation.
- Bilateral capillary occlusions involving the perifovea vessels as well as other isolated foci of occlusion in the posterior pole of the retina.
- Headaches due to papilledema.
- Mental confusion, loss of cognitive function, loss of memory, slowing of speech and hemiparesis due to “firm masses” and white, granular, firm lesions in the brain.
- Jacksonian seizures and grand mal seizure disorder.
- Progressive neurologic deterioration unresponsive to systemic corticosteroid therapy.
- Discrete, often confluent, foci of coagulation necrosis in the cerebral white matter with intermittent findings of fine calcium deposition within the necrotic foci.
- Vasculopathic changes involving both arteries and veins of medium and small caliber present in the cerebral white matter.
- Fibroid necrosis of vessel walls with extravasation of fibrinoid material into adjacent parenchyma present in both necrotic and non-necrotic tissue.
- Obliterative fibrosis in all the layers of many vessel walls.
- Parivascular, adventitial fibrosis with limited intimal thickening.
Genetics
The official name of the TREX1 gene is “three prime repair exonuclease 1.” The normal function of the TREX1 gene is to provide instructions for making the 3-prime repair exonuclease 1 enzyme. This enzyme is a DNA exonuclease, which means it trims molecules of DNA by removing DNA building blocks (nucleotides) from the ends of the molecules. In this way, it breaks down unneeded DNA molecules or fragments that may be generated during genetic material in preparation for cell division, DNA repair, cell death, and other processes.
Changes (mutations) to the TREX1 gene can result in a range of conditions one of which is AD-RVCL. The mutations to the TREX1 gene are believed to prevent the production of the 3-prime repair exonuclease 1 enzyme. Researchers suggest that the absence of this enzyme may result in an accumulation of unneeded DNA and RNA in cells. These DNA and RNA molecules may be mistaken by cells for those of viral invaders, triggering immune system reactions that result in the symptoms of AD-RVCL.
Mutations in the TREX1 gene have also been identified in people with other disorders involving the immune system. These disorders include a chronic inflammatory disease called systemic lupus erythematosus (SLE), including a rare form of SLE called chilblain lupus that mainly affects the skin.
The TREX1 gene is located on chromosome 3: base pairs 48,465,519 to 48,467,644
The immune system
- The immune system is composed of white blood cells or leukocytes.
- There are 5 different types of leukocytes.
- Combined, the 5 different leukocytes represent the 2 types of immune systems (The general or innate immune system and the adaptive or acquired immune system).
- The adaptive immune system is composed of two types of cells (B-cells which release antibodies and T-cells which destroy abnormal and cancerous cells).
immune system becomes part of the condition
During mitosis, tiny fragments of “scrap” single strand DNA naturally occur inside the cell. Enzymes find and destroy the “scrap” DNA. The TREX1 gene provides the information necessary to create the enzyme that destroys this single strand “scrap” DNA. A mutation in the TREX1 gene causes the enzyme that would destroy the single strand DNA to be less than completely effective. The less than completely effective nature of the enzyme allows “scrap” single strand DNA to build up in the cell. The buildup of “scrap” single strand DNA alerts the immune system that the cell is abnormal.
The abnormality of the cells with the high concentration of “scrap” DNA triggers a T-cell response and the abnormal cells are destroyed. Because the TREX1 gene is identical in all of the cells in the body the ineffective enzyme allows the accumulation of “scrap” single strand DNA in all of the cells in the body. Eventually, the immune system has destroyed enough of the cells in the walls of the blood vessels that the capillaries burst open. The capillary bursting happens throughout the body but is most recognizable when it happens in the eyes and brain because these are the two places where capillary bursting has the most pronounced effect.
Pathogenesis
The main pathologic process centers on small blood vessels that prematurely “drop out” and disappear. The retina of the eye and white matter of the brain are the most sensitive to this pathologic process. Over a five to ten-year period, this vasculopathy (blood vessel pathology) results in vision loss and destructive brain lesions with neurologic deficits and death.
Most recently, AD-RVCL (CRV) has been renamed. The new name is CHARIOT which stands for Cerebral Hereditary Angiopathy with vascular Retinopathy and Impaired Organ function caused by TREX1 mutations.
Diagnosis
Differential diagnosis
- Brain tumors
- Diabetes
- Macular degeneration
- Telangiectasia (Spider veins)
- Hemiparesis (Stroke)
- Glaucoma
- Hypertension (high blood pressure)
- Systemic Lupus Erythematosus (SLE (same original pathogenic gene, but definitely a different disease because of a different mutation in TREX1))
- Polyarteritis nodosa
- Granulomatosis with polyangiitis
- Behçet's disease
- Lymphomatoid granulomatosis
- Vasculitis
Treatment
Currently, there is no therapy to prevent the blood vessel deterioration.
History
- 1985 – 1988: CRV (Cerebral Retinal Vasculopathy) was discovered by John P. Atkinson, MD at Washington University School of Medicine in St. Louis, MO
- 1988: 10 families worldwide were identified as having CRV
- 1991: Related disease reported, HERNS (Hereditary Endiotheliopathy with Retinopathy, Nephropathy and Stroke – UCLA
- 1998: Related disease reported, HRV (Hereditary Retinal Vasculopathy) – Leiden University, Netherlands
- 2001: Localized to Chromosome 3.
- 2007: The specific genetic defect in all of these families was discovered in a single gene called TREX1
- 2008: Name changed to AD-RVCL Autosomal Dominant-Retinal Vasculopathy with Cerebral Leukodystrophy
- 2009: Testing for the disease available to persons 21 and older
- 2011: 20 families worldwide were identified as having CRV
- 2012: Obtained mouse models for further research and to test therapeutic agents